Is there a link between fatty liver and a lack of vitamin B12? What can you do about it?
Is there a link between fatty liver and a lack of vitamin B12? What can you do about it?
Fatty liver disease, specifically non-alcoholic fatty liver disease (NAFLD), has become a global health problem that affects millions of people without them knowing it. Typically ignored, Vitamin B12 deficiency can have serious effects on metabolism, brain health, and liver function. More and more doctors are looking at the possibility that fatty liver and a lack of vitamin B12 may be linked. This in-depth post looks into this connection and gives you measures you may take to fix it.
 Learning about Fatty Liver Disease: A Hidden Epidemic
Learning about Fatty Liver Disease: A Hidden Epidemic
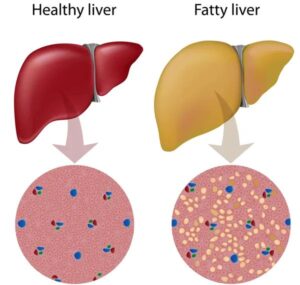
An improper buildup of fat in the liver cells is what causes fatty liver disease. There are two main types of fatty liver disease:
Fatty Liver Disease That Isn’t Caused by Alcohol (NAFLD)
NASH, or non-alcoholic steatohepat
NAFLD is not too serious in the beginning, but it can lead to liver fibrosis, cirrhosis, and hepatocellular cancer. People with NAFLD are more likely to have metabolic syndrome, obesity, insulin resistance, and type 2 diabetes.
Vitamin B12 is crucial for human health.
Vitamin B12 (cobalamin) is a water-soluble vitamin that is necessary for
Making red blood cells
Making DNA
Function of the nervous system
The metabolism of amino acids and fatty acids
If you don’t get enough of it, you could get neurological problems, megaloblastic anemia, cognitive loss, and high homocysteine levels, which is a known risk factor for heart disease.
Is there a link between a lack of vitamin B12 and fatty liver?
Yes, a new study shows that there is a strong link between NAFLD and low levels of vitamin B12 in the blood. There has to be additional research to prove that there is a direct cause-and-effect relationship; however, there are a number of ways that this possible link could work:
1. Poor storage and transport in the liver
The liver is where vitamin B12 is mostly stored. Liver cells in people with fatty liver disease don’t work right because of too much fat and inflammation. This makes it harder for them to store and release B12.
2. Problems with gut microbiota dysbiosis and absorption
NAFLD is associated with gut dysbiosis, which means that the bacteria in the gut are not balanced. This might make it hard for the small intestine to absorb B12.
Also, people with NAFLD may have irritable bowel syndrome, celiac disease, or SIBO (small intestinal bacterial overgrowth), all of which are known to make it harder for the body to absorb vitamin B12.
3. Metabolic syndrome and insulin resistance
Insulin resistance, which is a key part of the development of NAFLD, has also been linked to lower levels of Vitamin B12. Chronic inflammation and oxidative stress mess with how nutrients are used, which can cause subclinical deficiencies even when a person eats a regular amount of food.
4. Taking Metformin or Proton Pump Inhibitors (PPIs) for a long time
Many people with NAFLD and type 2 diabetes take metformin, and many with gastric reflux take PPIs. Both of these drugs are known to reduce the body’s ability to absorb vitamin B12, which makes things even more complicated.
 Signs that people with fatty liver may not be getting enough vitamin B12
Signs that people with fatty liver may not be getting enough vitamin B12
Fatty liver often doesn’t show any signs. If you have both liver and neurological symptoms, though, a lack of vitamin B12 could be a problem. Be careful of:
Constant tiredness and weakness
Hands and feet that feel tingly or numb
Problems with memory and brain fog
Skin that is pale or yellow
Glossitis, or a swollen and red tongue
Breathlessness
Changes in mood, such depression
Finding out if NAFLD patients have a vitamin B12 deficiency
A full assessment is needed to confirm a B12 deficiency in someone with fatty liver. These are some of the tools used for diagnosis:
Level of Vitamin B12 in the blood
Methylmalonic acid (MMA) levels go up when you don’t have enough B12.
High levels of homocysteine are common when there is not enough B12.
Complete blood count (CBC) to check for anemia
Liver function tests (LFTs) to check the liver’s health at the start
Ultrasound or FibroScan are examples of imaging tests that can be used to check liver fat.
What to Do: How to Handle Both Conditions Well
 1. Get the most out of your diet by eating foods high in vitamin B12.
1. Get the most out of your diet by eating foods high in vitamin B12.
Animal-based foods are the main sources of vitamin B12. People who have fatty liver and may not be getting enough B12 should eat more of:
Liver, meat, and chicken
Fish, especially salmon, sardines, and tuna
Dairy and eggs
Nutritional yeast (for vegetarians and vegans) and fortified grains
You may need to take oral or injectable B12 supplements if changing your diet isn’t enough. Depending on the person’s demands, methylcobalamin or cyanocobalamin are the best forms.
2. Fix problems with the gut and absorption that are causing the problems.
Taking care of your gut health is very important for NAFLD. Taking probiotics, eating more fiber, and cutting back on gut irritants like ultra-processed foods will help restore microbial equilibrium and make it easier for your body to absorb nutrients.
When someone has SIBO or IBS, they need focused treatment to fix the lining of their gut and get the most B12.
 3. Changes to your lifestyle to reverse fatty liver
3. Changes to your lifestyle to reverse fatty liver
A multimodal lifestyle strategy can stop early NAFLD and raise B12 levels:
Losing 7–10% of your total body weight can greatly lower the amount of fat in your liver.
Exercise (including aerobic and resistance training) makes insulin work better.
Diets that are low in carbohydrates and anti-inflammatory, like the Mediterranean diet, may be able to reverse NAFLD.
Stay away from alcohol and sugary drinks because they make liver fat build up faster.
4. Regular checkups and medical follow-up
People with NAFLD with a vitamin B12 shortage need to be watched all the time.
Check your B12 levels again every 3 to 6 months.
Get liver imaging done every year or as indicated.
Check for metabolic risk variables, including blood pressure, cholesterol, and glucose.
When should you think about taking B12?
If you do any of the following, think about taking B12:
If you have NAFLD/NASH and show signs of not getting enough B12,
Eat only vegetarian or vegan food
Take metformin or PPIs on a regular basis.
Have illnesses like Crohn’s disease, celiac disease, or surgery to lose weight.
You can supplement by:
Oral B12 pills (1,000 to 2,000 mcg each day)
B12 under the tongue for improved absorption
Intramuscular B12 shots, especially for people who are very deficient or can’t absorb it well
Conclusion: Finding a Balance Between Liver Health and Nutrition
More and more evidence is tying a lack of vitamin B12 to fatty liver disease. The effects are very important for long-term health. We may deal with both illnesses at the same time by taking a proactive approach that includes improving our diets, restoring our gut health, taking supplements, and changing our lifestyles.
Finding and treating vitamin B12 deficiency in people with NAFLD early on can help their neurological and hematologic health, and it may also help their liver repair and keep their metabolism in balance.
 https://analytics.google.com/analytics/web/#/analysis/p405220706
Skip to content
https://analytics.google.com/analytics/web/#/analysis/p405220706
Skip to content 
