The risk of developing fatty liver disease may be considerably increased by gallstones.
Introduction to Fatty Liver Disease and Gallstones
Fatty liver disease and gallstones are two common illnesses that can significantly affect general health. Fatty liver disease is defined by an excessive buildup of fat in the liver, whereas gallstones are hardened deposits of bile that develop in the gallbladder. Research indicates that gallstones may considerably increase the risk of developing fatty liver disease, despite their apparent unrelatedness.
This article examines the risk factors, effective prevention and management techniques, and the connections between various conditions.

Comprehending Gallstones
When bile components like cholesterol, bile salts, and bilirubin become out of equilibrium, gallstones can develop. These stones may or may not cause symptoms, and their sizes can vary.
Important Points:
Formation: Excess cholesterol, inadequate bile salts, or other bile imbalances can lead to the development of gallstones.
Types include pigment stones, mixed stones, and cholesterol stones.
Symptoms: While many people have no symptoms, gallstones that block bile flow can cause severe stomach discomfort, nausea, or vomiting in certain people.
Ultrasound imaging and symptom assessment are usually required for gallstone diagnosis.
Fatty liver disease: what is it?
Excess fat accumulates in the liver cells in fatty liver disease. It is mostly divided into two categories:
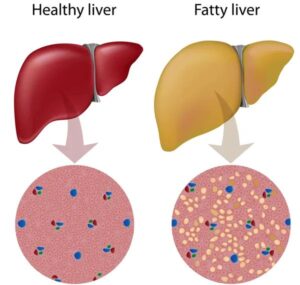
Poor lifestyle choices and metabolic problems are the main causes of non-alcoholic fatty liver disease (NAFLD).
Excessive alcohol use causes alcoholic fatty liver disease (AFLD).
Risks and Symptoms:
Symptoms are often absent in the early stages.
Cirrhosis, scarring, or inflammation of the liver may result from advanced stages.
The Role Gallstones Play in Fatty Liver Disease
Gallstones and fatty liver disease are linked by a number of mechanisms:
Risk factors that are common to both illnesses include poor diet, metabolic syndrome, and obesity.
Gallstones can cause bile flow disruption, which can result in fat buildup and liver damage.
Research Evidence: Studies show that fatty liver disease is more common in people with gallstones, especially if metabolic problems are also present.
Risk Elements Connecting the Two Conditions
People can take preventative action by being aware of common risk factors:

Obesity: Being overweight raises the risk of developing gallstones and accumulating liver fat.
Dietary Practices: Excessive use of processed foods and high-fat diets increases hazards.
Genetics: People may be predisposed to both illnesses due to their family history.
Strategies for Prevention and Management
A proactive strategy centered on prevention and efficient management is needed to address the connection between gallstones and fatty liver disease.
Dietary Modifications:
Choose a diet that is well-balanced and high in fiber, lean proteins, whole grains, and healthy fats.
Limit your consumption of processed foods, sugar, and saturated fats.
Include foods high in antioxidants, such as leafy greens, almonds, and berries.
 Frequent Exercise: Exercise lowers cholesterol, enhances liver function, and aids in maintaining a healthy weight. Every day, try to get in at least 30 minutes of moderate activity.
Frequent Exercise: Exercise lowers cholesterol, enhances liver function, and aids in maintaining a healthy weight. Every day, try to get in at least 30 minutes of moderate activity.
Medical Check-ups: For the early identification of concerns, routine testing for metabolic health markers such as blood sugar, cholesterol, and liver enzymes is essential.
Methods of Diagnosis
The management of gallstones and fatty liver disease depends on a prompt and precise diagnosis.
Imaging Methods:
Ultrasound is frequently used to measure liver fat and find gallstones.
CT or MRI scans are examples of advanced imaging that can offer in-depth information.
Blood Examinations:

Tests for liver function measure the levels of enzymes that signify liver stress.
Tests for glucose and lipid profiles are useful in determining the underlying metabolic issues.
Liver Biopsy: In extreme situations, a biopsy can determine the degree of damage and confirm fatty liver disease.
Options for Gallstone Treatment
The size of the gallstones and the intensity of the symptoms determine the course of treatment.
Non-Surgical Interventions:
Medication: Although the effects are gradual, bile acid tablets may dissolve tiny cholesterol stones.
Lifestyle Modifications: A low-fat diet helps reduce the symptoms of gallstones and stop them from getting worse.
Surgical Procedures:
The most popular method for removing the gallbladder and successfully preventing gallstone recurrence is laparoscopic cholecystectomy.
After Surgery: A nutritious diet should be adopted by patients to make up for any alterations in digestion.
How to Handle Fatty Liver Disease
It takes constant work to reverse or delay the progression of fatty liver disease.
Plans for Diets:
Emphasize meals that are low in carbohydrates and high in protein.
Steer clear of alcohol as it hastens liver damage.
Add omega-3 fatty acids, which lower fat accumulation and inflammation.
Weight Loss and Exercise:
Liver fat can be considerably decreased with moderate weight loss.
Resistance training promotes liver repair and enhances metabolic health.
Drugs and Surveillance:
For NAFLD, doctors may prescribe medications such as pioglitazone or vitamin E.
Frequent evaluations of liver function monitor progress and identify any issues.
Diet’s Contribution to the Prevention of Both Conditions
A healthy diet is essential for reducing the incidence of gallstones and fatty liver disease.
Foods to Incorporate:
For fiber and antioxidants, eat fresh fruits and vegetables.
lean meats, such as poultry, fish, and beans.
Nuts, avocado, and olive oil provide good fats.
Items to Steer Clear of:
Fast food and fried food.
sugary drinks and snacks.
Alcohol makes liver disease worse.
To guarantee proper bile flow and general liver function, hydration is equally important.
Changes in Lifestyle for Long-Term Health
A healthy lifestyle is essential for lowering risks and successfully treating fatty liver disease and gallstones.
 Controlling Weight:
Controlling Weight:
Rapid diets are not as effective as gradual, long-term weight loss.
By maintaining regular routines, try to maintain a BMI within the healthy range.
Reducing Stress:
Metabolic health can deteriorate due to prolonged stress.
Methods such as yoga, meditation, or mindfulness can enhance general well-being.
Habits That Are Sustainable:
Better results are guaranteed over time when long-term habits like meal planning, consistent exercise, and avoiding unhealthy snacking are developed.
Effects of Untreated Liver Gallstones
Liver health might suffer greatly if gallstones are not treated.
Problems Associated with Gallstones:
Jaundice and inflammation can be caused by blocked bile ducts.
Acute medical emergencies may result from gallstone pancreatitis.
Chronic Inflammation: Gallstone-induced chronic inflammation can harm liver cells, encouraging the buildup of fat and scarring.
Risk of Liver Failure: In severe situations, untreated gallstone problems may lead to irreversible liver failure, necessitating the possibility of a liver transplant.
The Value of Health Care Monitoring
The best possible treatment of gallstones and fatty liver disease is ensured by constant collaboration with medical specialists.
Collaboration with Physicians:
Personalized care plans are made possible by talking about risk factors and family history.
Following medical counsel improves recuperation and stops development.
Regular Screenings: Early indications of problems can be found with routine monitoring using imaging and blood testing.
Seeking Medical Assistance: Severe symptoms such as chronic pain, jaundice, or digestive problems require prompt medical attention.
Upcoming Studies and Developments
Better strategies to treat and avoid gallstones and fatty liver disease are still being investigated by ongoing research.
Novel Therapies:
sophisticated drugs that target the balance of bile acids and cholesterol.
surgical methods that are less intrusive for a quicker recovery.
New Diagnostic Techniques:
AI-driven imaging technologies enabling quicker and more precise detection.
blood test biomarkers that forecast the course of a disease.
Personalized medicine: Customized preventative and treatment strategies are made possible by an understanding of genetic predispositions.
In conclusion
Gallstones and fatty liver disease are linked, which emphasizes the significance of preventative health care. People can lower their risk of having these disorders by being aware of the common risk factors, symptoms, and preventative measures. Long-term health depends on establishing permanent habits, prioritizing a healthy lifestyle, and getting frequent medical attention.
FAQ 1. Can gallstones harm the liver permanently?
Indeed, gallstones that are left untreated have the potential to cause irreversible harm by blocking bile flow and generating persistent liver inflammation.
2. What are fatty liver disease’s early warning signs?
Common early indicators include fatigue, minor stomach pain, and high liver enzyme levels.
3. Can gallstones be cured by removing the gallbladder?
Although gallbladder removal stops gallstones from happening again, other digestive problems can still be avoided by changing one’s lifestyle.
4. Is it possible to reverse fatty liver disease?
Yes, fatty liver disease, particularly NAFLD, may frequently be reversed in its early stages with the right diet, exercise, and medicinal intervention.
5. How can I reduce my chance of developing both conditions?
Consume a balanced diet, engage in regular exercise, monitor your cholesterol levels, and schedule regular doctor’s checkups to lower your risk.
 https://analytics.google.com/analytics/web/#/analysis/p405220706
Skip to content
https://analytics.google.com/analytics/web/#/analysis/p405220706
Skip to content 
1 thought on “The risk of developing fatty liver disease may be considerably increased by gallstones.”